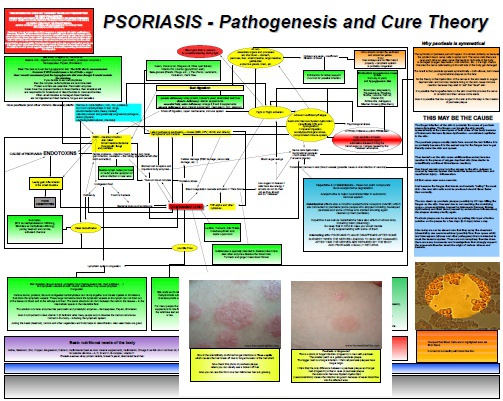
Obesity is Caused by Leaky Gut and Endotoxin Induced Inflammation
Even though obesity is considered as a risk factor of psoriasis the truth is that both conditions have usually the same underlying cause – endotoxin induced inflammation. Being overweight is considered as a problem of overeating rather than a real disease which should be addressed properly. Gaining the fat from eating excessive amounts of calories is not the same as gaining the weight (fat and water-weight) due to inflammation as it is present in obese people. During the inflammation the…