Psoriasis Severity is Correlated With the Fibrinogen Levels
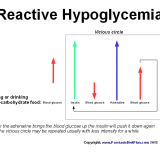
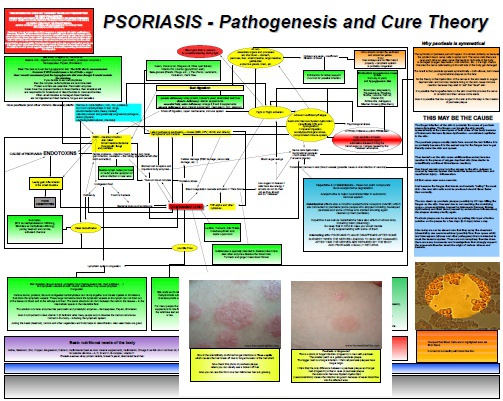
From the beginning of this blog I claim that psoriasis is caused by low oxygen levels in the body and skin. I say the cause or at least huge contributing factor is thick blood what causes bad blood flow mostly in the microvessels which are naturally so narrow that even one red blood cell must be really flexible to go through it. https://www.youtube.com/watch?v=UlAIHmv_0p8 Fibrinogen – inflammation and thick blood What role does the fibrinogen play in psoriasis pathogenesis? Well, fibrinogen…