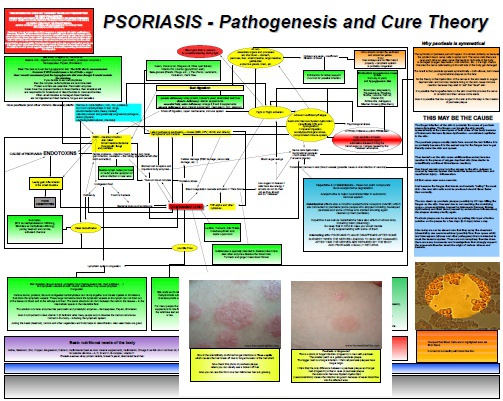
How High Cortisol Cause Psoriasis
Psoriasis sufferers are not the only who might benefit from reading this cortisol related article. Everybody who developed psoriasis or any other chronic health problem after a stressful period or event in his life might found following information very useful. This article about cortisol and psoriasis will be a little bit difficult to understand completely so you may want to read it twice but I think it is worthy to understand the ideas and evidence presented here in the next…