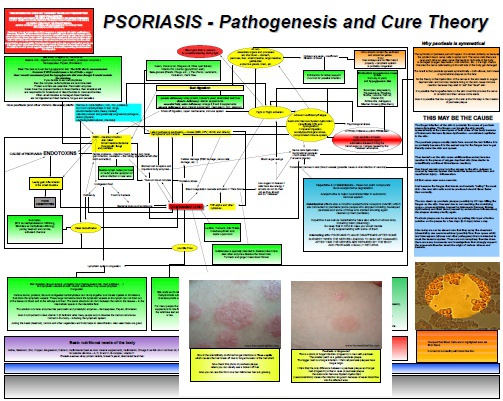
Psoriasis And Seborrheic Dermatitis Are Both Caused by Antibiotics Induced Fungal Overgrowth
If you are one of those close-minded people who thinks that psoriasis is something entirely different than seborrheic dermatitis and surely not curable with fluconazole you may want to avoid reading this article. In this post I will present you a testimonial of one seborrheic dermatitis sufferer who shared his experiences with his diagnosis and how it developed following the antibiotics treatment. His words speak for themselves and if you know how stubborn and health destroying the yeast and fungal…