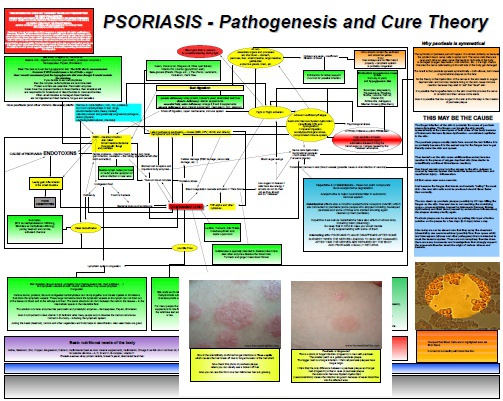
Psoriasis Is Caused By Bad Digestion
Bad digestion is probably the most common and significant cause of psoriasis. Gut health, stress and psoriasis all go hand in hand. Bad digestion leads to huge inflammation which creates the symptoms of psoriasis and other chronic health problems. We all know that stress can significantly impair the blood flow throughout the body. I published the blog posts and mostly video about this issue and how it relates to psoriasis before. Digestion, Stress and Psoriasis Adrenaline as a fight-or-flight hormone…