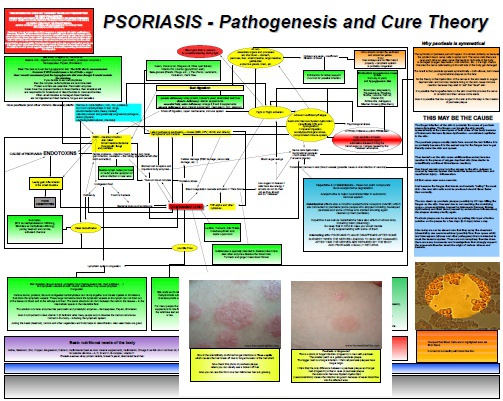
How AIDS Leads To Psoriasis
Psoriasis is reported to be more prevalent in HIV infected population compared to HIV negative population. What is a paradox the scientists are trying to resolve? How is it that immunocompromised patients develop the disease which is considered to be caused by overactive immune system…? There are only two possible reasonable explanations which come to my mind: Psoriasis is not a disease of immune system in the first place or HIV infection does not cause the breakdown of all immune…